Response Essay Writing Help

Reproductive system is one of the essential parts of human body that helps in the production of offspring.
Since the fertilization in human is internal and involves two individual of different sexes, male and female, hence reproductive system of both also varies involving different organs.
Female reproductive system: all the parts of body that are important for the process of reproduction in female constitute female reproductive system. On one hand male reproductive system produces the sperm whereas on the other hand female reproductive system produces egg. Therefore, the organs and their functions are completely different with respect to male.
Histology of female reproductive system
Important organs involved in reproduction along with their histological description are as follows:
1. Ovaries: these are the paired gland that are homologous to the testis in male. It consist of different parts:
- Germinal epithelium: it is the layer of simple epithelium that consist the surface of ovary.
- Tunica albuginea: it lies below the germinal epithelium and is white in color. It is made up of irregular connective tissue.
- The ovarian cortex: it lies deep to tunica albuginea that and consist of ovarian follicles.
- The ovarian medulla: it lies deep to cortex and consist of lossely arranged connective tissue along with blood vessels and nerves.
- Ovarian follicle: these are the basic unit of female reproductive system that lies within the cortex. Itconsist of oocytes at its various stages of development.
- Mature/ graffian follicle: it is large and is filled with fluid, it is the stage where secondary oocyte is just about to release.
- Corpus luteum: it is a yellow body, a left over after the process of ovulation is completed. It secretes different hormones until it degenerates into corpus albicans.
Reproductive system in female Assignment Help By Online Tutoring and Guided Sessions at AssignmentHelp.Net

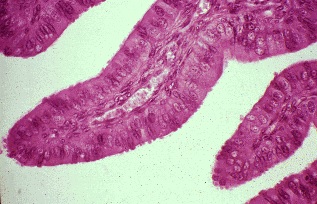
2. Uterine tube: it extends laterally from the uterus. These are composed of three layers:
- Serosa: it is the outermost layer of uterine tube that is composed of thin layer of connective tissue and mesothelium.
- Muscularis: it is the middle layer and is organized quite differently then inner and outer layers. It has thick ring of smooth muscle on the inner surface and thin region of longitudinal smooth muscle in the outer layer. Thus, the coordinated action of both this part helps to push fertilized ovum towards the uterus.
- Mucosa: it is the inner layer of uterine tube that have many thin longitudinal folds that are complex in ampulla and get lowered down or less in isthmus. The lining of mucosa consists of ciliated and non- ciliated cells. Ciliated simple columnar cells consist of ciliated simple columnar cells that help to move fertilized ovum to the uterus and also the non- ciliated cells called peg cells that secrete the fluid that supply important nutrition to the ovum.
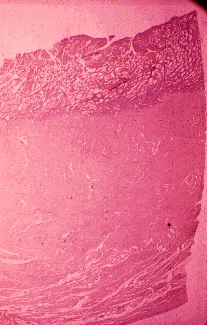
3. Uterus: it is pear shaped organ that consists of 3 layers:
- Perimetrium: it is composed of simple squamous epithelium and aerolar connective tissue. It covers the entire posterior surface of uterus and only some part of anterior surface. Anteriorly, it covers the urinary bladder thus forming vesicouterine pouch, whereas on the posterior surface it covers rectum, thus forming a deep pouch between uterus and urinary bladder called rectouterine pouch.
- Myometrium: it consist of thick muscle layers that are thickest in fundus and thinnest in cervix.
- Endometrium: it is the inner layer of uterus, whose innermost layer consist of simple columnar epithelium, an underlying region of lamina propria. This layer is divided into sublayers of stratum fuctionalis that lines the uterine cavity and the depper layer stratum basalis, that give rise to new stratum functionalis.
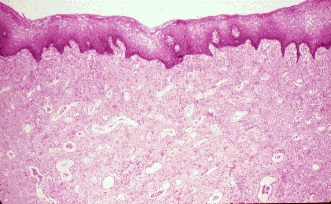
4. Vagina: it is tubular and extends from exterior of the body to the uterine cervix. It consist of nonkeratinized stratified squamous epithelium and aerolar connective tissue. The vaginal wall consist of different layers:
- Inner mucosal layer: it consists of number of folds called ruggae and lined with stratified squamous epithelium. Connective tissue papillae from the underlying lamina propria project into epithelial layer, therefore nuclei can be seen throughout the thickness of epithelium.
- Intermediate mucosal layer: it has outer longitudinal layer and inner circular layer in which outer layer is much thicker than the inner layer.
- Outer adventitia: it consist of aerolar connective tissue and helps in anchoring of vagina to the corresponding organs.
5. Vulva: it is external genitelia of female that consist of mons pubis, labia majora, labia minora, clitoris and vestibule. The mons and labia majora are covered by keratinized stratified squamous epithelium including hair follicle, sebaceous gland and sweat gland. Labia minor is covered with non- keratinized squamous epithelium with no or rare sweat gland. The clitoris is covered by non keratinizing squamous epithelium and contains stroma that is rich in erectile vascular structures.
Physiology of female reproductive system
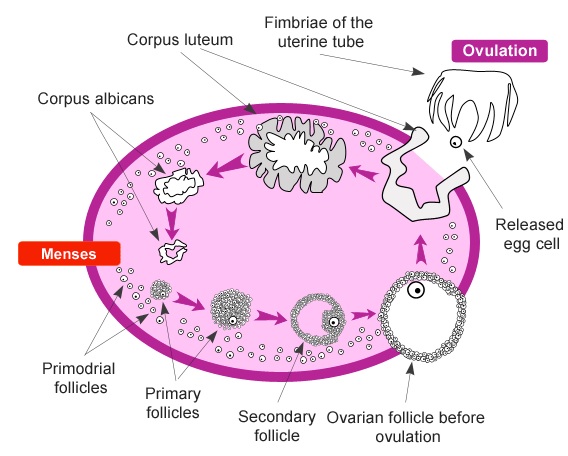
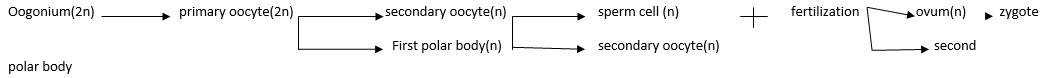
Oogenesis, formation of female gametes begins even before the birth of a girl child. During the fetal development primitive germ cells migrate to the ovaries, thus differentiating into oogonia. Then the oogonia divide by mitosis producing germ cells. Among many some of the germ cells some become larger forming primary oocytes that enter prophase of meiosis 1 but at this stage they get arrested. At the time of birth, many oocytes are present in the ovary but as the women reach the age of maturity only few oocyte are present that gets mature rest all the oocytes degenerate. After puberty, every month until a woman menopause, many primordial follicles develop into primary follicle that has primary oocyte inside it and is surrounded by several layers of cells. These cells are made of cuboidal and low- columnar epithelium, called granulose cell. Slowly, it starts to grow in size. Primary follicle gets surrounded by zona pellucid and theca follicular as it develops. Slowly, it develops into secondary follicle where theca differentiates into theca externa and theca interna. Beside this, a fluid filled cavity called antrum slowly starts to develop thus increasing the size of the secondary follicle. Added with this, any granulose cells that are attached to zona pellucida are now called corona radiate. As the secondary follicle grows in size, it is now called graffian follicle. At this very stage, primary oocyte completes its meiosis 1 forming two haploid cell of unequal size, in which the smaller is called first polar body and the other having maximum cytoplasm is called secondary oocyte. Now, meiosis 2 starts and again gets paused at metaphase stage thus continuing with the process of ovulation. Ovulation is the process when secondary oocyte is released from mature graffian follicle. Now the expelled material, that is secondary oocyte with first polar body and corona radiate, reach pelvic cavity and finally to uterine tube. If no fertilization occurs then cells degenerate whereas if sperm reaches uterine tube of female and penetrates the secondary oocyte then meiosis 2 resumes and fertilization occurs forming secondary polar body and ovum that undergoes fertilization to form zygote. Thus, from millions of oognia, finally one ovum is formed in female reproductive system.